Bwindi Community Hospital
Bwindi only opened its doors as a hospital in 2003.
It is positioned close to the Bwindi Impenetrable forest to be accessible to the Batwa people who were displaced from the forest when the government decided the gorillas should take priority, regardless of the impact on the people displaced.
This location means that the hospital is literally at the end of the road to the forest, which does not facilitate access to the rest of the district. The hospital does gain support from tourists who come to visit it, while coming to go on a trek to see the gorillas.
Bwindi Community Hospital has a strong community focus and a vision to create a healthy community in the district, so they have worked hard with our support to develop mental health services out in the community.
First visited by Jamie’s Fund in 2013

Benedict Medical Centre, Luzira, Kampala
This Health Centre IV consists of two 3 storey buildings south of the city centre. It functions as a small general hospital of 66 beds serving the urban poor in the vicinity. Dr Fred Adea is the Medical Director. They have no specialist mental health (MH) staff. They are increasingly concerned by the levels of substance abuse they see.
They recognise the importance of doing more to address mental ill health. They hold outreaches when resources permit, which consists of ‘taking the hospital to the community’ for a day. People living in slum conditions nearby are screened and treated for free. All staff are involved, as the outreach also includes a community clean-up!
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who are planning to roll out training in the hospital and nearby Health Centres. They have also identified a staff member to start PCO (Psychiatric Clinical Officer) training, sponsored by Jamie’s Fund.
First visited by Jamie’s Fund in 2019.


Bishop Caesar Asili Hospital, Luweero
This hospital is north of Kampala, on the edge of the town of Luweero, and offers the usual services of a local general hospital. Dr Charles Lwanga is the medical director, and Sister Ernestine Akulu is the hospital administrator. There are no specialist MH staff. They treat many patients for epilepsy. They recognise that people with mental ill health come with physical symptoms to Outpatients and other departments, but can be overlooked unless the symptoms are very obvious. They treat and manage people who have attempted suicide.
They ‘have a community hand, already’ working with orphans, HIV/AIDS, income generation for vulnerable households, and a COOP savings scheme.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who are planning to roll out training in the hospital and nearby Health Centres.
First visited by Jamie’s Fund in 2019.


Bukwo Health Centre IV
Bukwo HC IV is a fairly small health unit run by the Catholic church.
Bukwo is a small town in a relatively poor area. It is the administrative centre for the district which has been made a separate district relatively recently. It is to the east of Mt Elgon bordering on Kenya.
There is a government HC IV in the town as well
They have a PCO and a psychiatric nurse and are interested in developing better mental health services. Demand appears to be low.
Staff have attended mhGAP training and plan to hold a rollout workshop once lockdowns allow.
The access road to Bukwo is terrible and only passable by 4×4 only. There is an alternative road along Kenyan border which is a little better but longer. Construction of a new road has started but it is not clear when it will be complete.
First visited in 2019


Holy Family Virika Hospital, Fort Portal
This well-cared for general hospital has the usual services, and is situated in Fort Portal town, serving an urban population. Dr Jubilee is the MD, and Sister Mary Magdalene is Director of Nursing. The only mental health specialist is Diploma Nurse Innocent Mwebaze, who teaches part time in the School of Nursing. They recognise people with mental ill health in Outpatients, Maternity and elsewhere, and they treat people who have attempted suicide. They wish to be able to do so much more for their community.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who are planning to roll out training in the hospital and nearby Health Centres.
First visited by Jamie’s Fund in 2019.


Kabarole Hospital, Fort Portal
Kabarole is the second oldest hospital in Uganda (115 years) and serves an urban population in Fort Portal with the usual range of services. Dr Mugisha Edward is the MD, Stephen Waako is the Hospital Administrator, and Asio Betty Kasoro is the Principal Nursing Officer. Betty was a Diploma MH nurse, before retiring and coming to her post in Kabarole. They have no other MH specialist staff.
There is no regular MH clinic in the hospital, they do try to follow up people who have attempted suicide, or refer them on. They are seeing an increasing number of people with significant MH needs in Outpatients and other clinics.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who are planning to roll out training in the hospital and nearby Health Centres.
First visited by Jamie’s Fund in 2019.


Kagando Hospital
Kagando Hospital is a well-established Church of Uganda Hospital in the west of Uganda near Kasese. It is not far from the border with the DRC. The hospital was started in the 1960’s and has grown and developed over the years.
They have two nursing staff trained in psychiatry and have worked to develop a community mental health service, but this has been disrupted by COVID and staffing changes.
First visited in 2016

Kisiizi Hospital
Kisiizi hospital is a long standing hospital in southwest Uganda near Kabale. It was the first of the Church of Uganda hospitals to start a mental health service in 1998, and to have an inpatient service for those with mental illness.
They provide a good mental health service based on admission to the ward and have three clinics in the community. They are interested in doing more but so far have not been able to develop much work in the community as they would like.
First visited in 2010


Kilembe Mines, Kasese
The Hospital was established 1951 to meet the needs of mine workers at the copper mines, their families and the wider population around. Unfortunately their hospital was destroyed by flood waters in March 2020.
They have re-established the hospital facilities in Kasese until they can rebuild nearer the mines again.
They have two PCO’s and are interested in developing services for people with mental illness in the community.
They have two staff trained in mhGAP funded by Jamie’s Fund and ran a rollout workshop in April 2021.
JF partner since September 2019
St Josephs Hospital, Kitovu (UCMB)
The hospital sits on a rise on the outskirts of Masaka town, and has the usual range of services of a general hospital, plus a fistula service, which is busy. There are 66 nursing staff. Dr Alfred Lumala is the MD, Sister Christine is the Director of Nursing. They have no MH specialists on the staff. There is no MH clinic or outreach clinic. They recognise there are people with mental ill health on the wards, and in Outpatients, who often remain overlooked and untreated. They are eager to change this.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who will plan to roll out training in the hospital and nearby Health Centres.
First visited by Jamie’s Fund in 2019.


Kumi Hospital
This is a former leprosy hospital a bit out of town and spaciously set out. The hospital management is supportive of developing a mental health service.
As a result of the MH GAP training, they have MH representatives in most parts of the hospital.
There is a PCO who visits monthly, seeing 8-10 people a week in his clinic. Most of them have epilepsy. As usual, the cost of medications is a significant issue.
Jamie’s Fund is sponsoring one of their registered nurses to train as a PCO.
They have been partners since 2018.


Lubaga Hospital, Kampala
This hospital opened in 1899 and so is one of the longest established hospital in Uganda. There are currently 250 beds. It is classed as a general hospital but in 2016 it was decided to plan to become a regional referral unit and so increase the specialisms in the hospital. This would include psychiatry.
Although there are no MH qualified staff at present, there is considerable interest and energy in developing a mental health service. They have run two mhGAP workshops mainly with staff from the hospital, and have a group that meets monthly to discuss how to take things forward.
They are keen to do more in the community and have run three community leaders’ sensitisation workshops to begin to address the stigma and lack of awareness in the community.
They have been partners since 2019.


Benedictine Eye Hospital, Tororo
The hospital was started as an eye clinic in a shipping container in 1986 by Father John.
The ophthalmology work has continued to expand over the years. It is now regarded as a national resource and a tertiary referral centre for the Eastern region. They have eye clinics over the region.
They have a well-established community-based rehabilitation programme. There are four in the team: Julius an OT, Brenda RMN, an orthopaedic clinical officer and a physiotherapy assistant. They assess people with disabilities. Those that are blind are treated if possible, orthopaedic problems are referred for surgery if appropriate, those with epilepsy are put on treatment and maintained. They try and rehabilitate those with other physical issues.
They have 11 mobile clinics which they go out to on motorbikes. Each clinic is run every two months. They have around 200 people with epilepsy on their register. They would like to expand the mental health component of their work and coordinate with other mental health services in the area.
Jamie’s Fund have sponsored the training of two staff in mhGAP and they are about to run a rollout workshop.
First visited in 2019.

Nkozi Hospital, Equator
Nkozi is a small District General Hospital, with the usual range of Outpatient and Inpatient services, situated near the Equator, just off the main road to Masaka. They also treat inmates from the nearby prison. There are 67 nurses and midwives. Dr Criscent Tumuhaise is the MD, Sister Harriet Baker is the Director of Nursing.
There is a part time PCO, Beningia Nabona, who works 2 days at Nkozi and 3 days at the nearby Government Hospital. They occasionally admit MH patients to a general ward. There is no regular MH clinic, but the PCO assesses and treats those who attend other clinics, about 100 patients in 6 months
They are keen to develop services because of unidentified and unmet need. They wish to train general staff to spot mental illness in patients. They really want to change the culture, to have a ‘vibrant MH clinic’!
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who are planning to roll out training in the hospital and nearby Health Centres. They have also identified a staff member to start PCO (Psychiatric Clinical Officer) training, sponsored by Jamie’s Fund.
First visited in 2019.


Ruharo Hospital, Mbarara
Ruharo is a small community hospital on the outskirts of the town of Mbarara, with a specialist eye centre adjacent. When we visited, there were no trained mental health staff, and no regular clinics for mental health. However, Medical Clinical Officer Patrick Barigye and Registered General Nurse Miria Tumuheki had always taken an interest in patients attending the hospital who turned out to have mental ill health. Patrick and Miria had attended the first mhGAP Train the Trainer course funded by Jamie’s Fund, and began to convince their colleagues that things had to change.
Funded by Jamie’s Fund, they have since carried out an mhGAP rollout programme for staff in the hospital and nearby Health Centres. Miria has also started PCO (Psychiatric Clinical Officer) training, sponsored by Jamie’s Fund.
First visited in 2018.

Rushere Community Hospital (UPMB)
Rushere is a compact 100 bed general hospital serving a largely rural community, north of the road between Masaka and Mbarara. Dr Sunday is the MD. Ruth Nanteza is currently studying to complete her MH Nursing Diploma. She returns to work at Rushere in the holidays, but otherwise Medical Officer Johnson Agaba covers the MH patients. There is no regular MH clinic specifically and the current service derives mainly from people presenting at outpatients or admitted with other conditions. An acute concern for the hospital is attempted suicide. Ruth or Johnson see these patients and try to follow them up. They are also asked regularly to assess the capacity of prisoners to stand trial.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who are planning to roll out training in the hospital and nearby Health Centres. There is a genuine motivation to positively develop MH services for those in need of them.
First visited by Jamie’s Fund 2018.

Rushoroza Hospital, Kabale
JF partner since October 2019
The hospital is on the road south from Kabale towards the border with Rwanda at Katuna. It is a small hospital only upgraded from a large health centre in 2018. It was started in 1963. There are plans to develop into a larger hospital, but it isn’t clear where the funds will come from
Dr Martin, the medical director, is enthusiastic They have not started mental health services yet. They have just run an MH GAP rollout workshop as a first step to developing more of a service.
JF partner since October 2019

Rwesande Health Centre, Kasese
This is a large health centre north of Kasese in a fairly rural area and it is under the supervision of Kagando C0U Hospital. The in-charge was supportive of developing a mental health service. There is a PCO there who sees some patients.
Two staff have been trained as mhGAP trainers and they are planning to run a mhGAP rollout out workshop.
First visited in 2018.

Mukono Hospital,
This is a busy hospital in Mukono, which is one of the satellite towns of Kampala.
The medical director, Dr Simon Nsingo, is very supportive of developing mental heatlh services. They have a general clinical officer who is keen to lead the development, a mental health nurse and a volunteer PCO. They have a weekly mental health clinic in the hospital and are about to start four community clinics, with support from Jamie’s Fund.
One of their nurses is being trained as a PCO. Once she has completed the training she will be able to help to lead the service.
First visited in 2019


St Charles Lwanga Hospital, Buikwe (UCMB)
This 95 bed general hospital, situated off the Jinja Road to the east of Kampala, serves a poor rural population with reportedly very strong traditional beliefs. Dr Sharon is the MD, and James Kazungu is the Hospital Director, SNO is Sister Rona Nsamba. There are no MH specialists among the staff and there is no MH clinic, they tend to see people with epilepsy and mental ill health on first presentation and refer elsewhere for treatment.
They recognise that MH has been a neglected area. Their plans are to include MH in their twice monthly ‘consolidated outreaches’.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who have already rolled out training in the hospital and nearby Health Centres.
First visited by Jamie’s Fund in 2019.

Uganda Martyrs Hospital, Ibanda (UCMB)
This well cared for general hospital is situated at the edge of Ibanda town, providing the usual range of outpatient and inpatient services. There are 55 nurses and midwives, 79 professional staff in total. Dr Emmanual Byaruhanga is the MD. There is one Certificate level MH nurse, Innocent Mujuni, who teaches in the school of nursing, as well as his clinical work. There is no regular specialist MH clinic.
Dr Emmanual has a brother with severe mental ill health, and so has some personal experience, and knows how families struggle. They are keen to do more to address mental health needs locally.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who are planning to roll out training in the hospital and nearby Health Centres. They have also identified a staff member to start PCO (Psychiatric Clinical Officer) training, sponsored by Jamie’s Fund.
First visited by Jamie’s Fund in 2019.

St. Francis Hospital, Buluba
The Hospital started in 1935 as a leprosy hospital and it has gradually developed from there. It retains a specialism in dermatology, which is recognised nationally. People disfigured by leprosy still live there as they are rejected by their own community but they are accepted locally.
It is relatively isolated, perhaps due to its origins and is not far from the shore of Lake Victoria. It was recognised as a hospital in 2003 and has gradually developed more services since.
Funding for the hospital is not easy. 40% of funding comes from the sale of sugar cane they grow.
They have an enrolled mental health nurse Rose pictured with Sister Proscovia. They would like to do more to raise the profile of mental health both in the hospital and the community
They have two staff trained as trainers in mhGAP and plan to run a rollout workshop to train others in the community, nearby health centres and hospital.
JF partner since 2019


St Francis Hospital, Nkokonjeru
This well-cared for general hospital of 100 beds serves a poor rural community to the east of Kampala, at as low a cost as they can manage. They supervise 20 small Health Centres. Dr Okello Lenard is the MD, and Sister Priscilla Mukiibi is the Hospital Administrator. There is one Diploma level MH nurse, Joel Mulabbi.
There is no regular MH clinic, but Joel helps with MH patients coming to Outpatients. There are also many attending with epilepsy, who are referred on for treatment. MH patients are identified and treated in the relatively new community outreaches. At present they have little capacity for follow-up.
Funded by Jamie’s Fund, they now have two staff trained as mhGAP trainers, who will plan to roll out training in the hospital and nearby Health Centres.
First visited by Jamie’s fund in 2019.

St Pauls Health Centre IV, Kasese
St Paul’s is a large HC which functions as a small hospital in Kasese town, with inpatient and outpatient services. Sudaat Alihabwa is an experienced PCO who had recently joined the staff in 2018, and was beginning to develop a MH service. She had benefitted from attending the first mhGAP Train the Trainer course funded by Jamie’s Fund.
Since then she has participated in collaborative meetings with MH staff from Kisiizi, Bwindi and Kagando hospitals for skill sharing and peer supervision, with the costs covered by Jamie’s Fund, and has rolled out an mhGAP training programme to her colleagues at St Paul’s, likewise.
First visited by Jamie’s fund in 2018.

St Stephens Hospital/HCIV, Mpererwe, Kampala
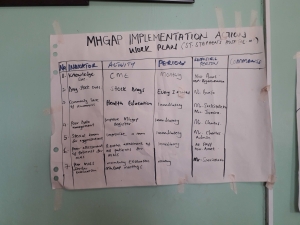
This is a small general hospital with a big heart, serving the urban poor in the north side of the city. Dr Catherine Nakibuule is the MD, and Olivia Nangendo is the Hospital Administrator. Reagan Amwesiga is the Clinical Officer who has taken an interest in MH, and trained as a mhGAP trainer. Maureen Kajobe is the Counsellor, and now also a mhGAP trainer. Reagan has incorporated MH community sensitisation in existing outreaches and medical camps, and has been building contacts with community and church leaders. Cost of treatment is a significant barrier locally.
Dr Catherine admits that they were not fully aware of the burden of mental ill health until more recently. They recognise the need to integrate MH with other services. Their plans (see chart) include the development of a regular MH clinic.
Jamie’s Fund has funded the training of Reagan and Maureen, as well as the two rollout training programmes they have facilitated for staff from the hospital and nearby Health Centres. St Stephens has also identified a staff member to start PCO (Psychiatric Clinical Officer) training, sponsored by Jamie’s Fund.
First visited by Jamie’s fund in 2018.

Cheshire and Wirral Partnership NHS Trust (CWP)
CWP staff worked with the mental health staff at Kisiizi Hospital using a multi disciplinary approach between 2010 and 2015 . This included staff visiting in both directions and learning from each other. Staff from UK were impressed by how much can be done with relatively few resources, and the consistently warm welcome all patients receive whenever they come to the hospital. The challenges and expectations are different in our two countries and the visitors have enjoyed the inter-cultural exchanges.

Diversity Travel
Diversity Travel has been supporting the new community mental health programme at Bwindi Community Hospital over the last three years, working closely with Jamie’s Fund.
Diversity Travel is an award-winning travel management company, based in Manchester, UK . The company, founded by Ugandan-Asian Harish Sodha, has worked helping charities to do their vital work around the globe for over 30 years. To mark Diversity’s landmark tenth anniversary, the team wanted to find a way to help people with mental illness in rural Uganda.
They are excited to work with Jamie’s Fund as they appreciate both the crucial work we do, as well as the transparency in the way funds donated are used directly by the hospital.”
Thank you
We are indebted to JMP Architects in Lancaster for all their work designing the new centre at Kisiizi and working with us to create a design that looks good and is appreciated by the patients and staff .
The Jamie’s Fund logo was designed by Amanda Gray Makinson and we appreciate her skill, and the ongoing permission to use it.
The plaque in memory of Jamie and proudly displayed at the entrance of the Ahamuza Centre in Kisiizi was generously donated by Peter Morris and Morris Memorials. It is shown in Avril and Jim’s photo on their “About Us” page.
The cover design of the “Cooking with Panache” cook book was created by Eddie Vine and we are grateful for gift of this.
Ed Lamb of Dupe Creations has creatively and willingly designed this website and continues to support its development.
