Jamie’s Legacy – Reflections by Jamie’s parents
As Jamie’s Fund draws to a close we have been reflecting on the wonderful way that Jamie’s life has touched so many others in the UK , Uganda and beyond. When Jamie died in 2011 our lives became unrecognisable, everything looked different and the sadness and pain was overwhelming. Yet even in our darkest hours we were certain that Jamie’s life had meaning beyond the four years that he was with us . We also knew that it was our job along with our friends in the UK and Uganda to figure out what this was and make sure his legacy was realised. People started to give money and we saw the potential for good things to come from establishing a small charity in Jamie’s name. We were supported by amazing people with greater knowledge and skills than us to set up Jamie’s Fund in 2013. Those people became trustees and advisors to Jamie’s Fund and have continued to this day, we will be forever grateful for their support.
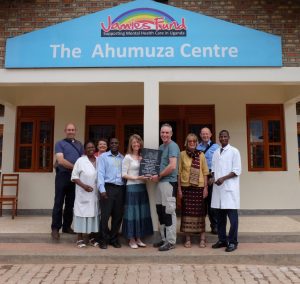
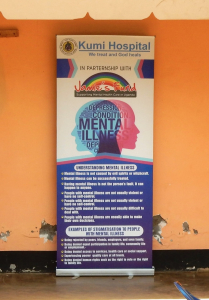
The charity initially worked with Kisiizi Hospital to design and build the Ahumuza Mental Health Centre. The formal opening of the centre in 2017 was an incredibly joyful and yet poignant event. Joyful because it is a very special place with amazing people bringing hope and mental health care to many. Poignant because it was our first visit to Kisiizi since we had been there with Jamie. We were comforted and strengthened by the sensitivity and the warmth of the welcome we received from the people of Kisiizi. It was a very moving experience.
After reaching our initial fundraising target money still kept coming to us, often from unexpected generous donations and legacies but also from epic fundraising efforts. It was heartening to see so many people having been inspired by Jamie’s story and the work of the charity to do such challenging things for sponsorship money. From non-runners training for and completing half and full marathons to people afraid of heights abseiling down Halkyn church tower. We were buoyed emotionally and the charity buoyed financially by the efforts people made.
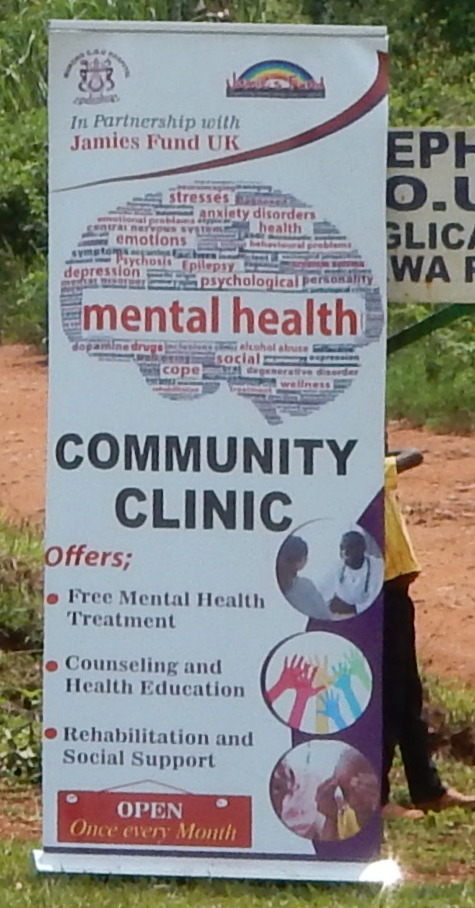
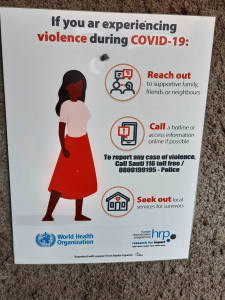
We had realised early on that our resources would have greatest impact by focusing on community based projects rather than just focusing on buildings. Our talented colleagues in Uganda worked with us to support individual mental health staff training as well as rolling out MHGap training across Uganda and also developing sensitisation training for village leaders. We began with a partnership with one hospital in South West Uganda and this has grown to a partnership with 25 hospitals across the whole of Uganda. Such reach and impact in Jamie’s memory is way beyond any hopes we had in our wildest dreams at the outset.

As a very small team, we always knew that we couldn’t continue indefinitely and that we needed to carefully choose a time to bring the work of Jamie’s Fund to a positive end. We made the very difficult decision to work towards closing the charity at the end of this year and were sad to have to let our partners in Uganda know as well as all our other supporters.
Our most recent trip to Uganda was incredibly uplifting and brought home the extent of which Jamie’s life has touched others. This includes the organisations we have encouraged and supported to develop mental health services, the individual mental health staff that we have supported with training and the people and communities that have directly and indirectly benefited from the mental health care provided by Jamie’s Fund’s partners.
During the first week of the visit we ran a professional development conference for thirty key mental health professionals that we have supported over the years. Their calibre and commitment was very striking and it was a very full and productive learning and networking week. Whilst there was sadness when we broke the news about Jamie’s Fund closing there was also much hope because within twenty four hours the group had rallied and made plans to set up their own organisation to ’Keep the mental health movement going’. We began to realise that our stepping away at this time was creating space for others who are now ready to step forward and take the work forward.

This theme continued during the second and third weeks of our trip when we made visits to hospitals and health centres that we have partnered. We were warmly welcomed and shown extensive progress. Time and time again we were thanked for the support and encouragement we had provided and reassured very firmly that the work will continue. Such commitment and enthusiasm confirmed to us that the time is indeed right for us to let go and make space for our very capable and enthusiastic Ugandan friends to take forward the work.
Jamie would have turned 16 this year and there’s not a day goes by where we don’t miss him and wish that he was still with us. This visit, however, was very special, it brought us to a new place of peace and acceptance. We now have the comfort of knowing that Jamie’s legacy has been fully realised and that countless people have been and will continue to be touched by his life, even if they don’t know his name.
We would like to sincerely thank everyone who has been involved over the years, none of this could have happened without your support. Having witnessed the progress of mental health care over the years and knowing the calibre of today’s practitioners and leaders, we are confident that mental health care in Uganda will continue to go from strength to strength. We look forward to seeing this happen because this certainly isn’t good bye. We look forward to visiting our friends in Uganda in the future and providing encouragement where we can.
Jamie’s Fund may close but Team Jamie is still very much around.
Jim and Avril Devaney, Jamie’s Parents
December 2023