In the UK we occasionally ask the doctor to visit us at home, if we are particularly ill. In Uganda a home visit from the doctor would be very unusual, certainly outside a city.
In rural areas your options are limited. There may be a local traditional healer but if you want to use “so-called” Western medicine then you and, if it’s really serious, your relatives will have to find your way to a local Health Centre or Hospital. For those with severe mental illness this may mean a long distance to travel. The cost of travel and the possibility of significant medical expenses, as well as the cost of time away from home, is all money that most people simply do not have.
In response to the mental health need, Jamie’s Fund is supporting a number of community projects in which medical teams visits outlying villages or homes to meet patients and their families. In many cases this is far more cost-effective than expecting patients to travel to find help.
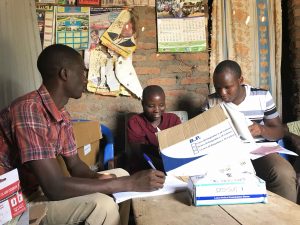
The community mental health teams supported by Jamie’s Fund are often held in villages, either in a health centre or in a convenient open space. Sometimes, however, the clinic is held in someone’s home. When Linda Shuttleworth and Hugh Burgess visited Kagando Hospital in November they were privileged to observe one such home visit.
A couple had opened their home and five people walked, some for many miles, to meet the health team there. The PCO (Psychiatric  Clinical Officer) led the clinic and dicussed each person’s health with them. A second nurse was there to manage the medicines and to ensure that each patient received what was prescribed.
Clinical Officer) led the clinic and dicussed each person’s health with them. A second nurse was there to manage the medicines and to ensure that each patient received what was prescribed.
What would surprise us, is the openness with which clinics are often held. “Community Medicine” can mean just that! There may be fifteen or twenty people gathered round the patient who are then party to the whole discussion. While this may seem alien to us, this openness can also be helpful. Not only does the community understand what the issues are with the patient but there is also a breaking down of barriers to treatment. As people become more aware of how mental illness can be treated, they spread the word to others and it becomes more acceptable to seek help.
The community health projects funded by Jamie’s Fund are now reaching several hundred people with mental illness or epilepsy, who are being treated much sooner than was previously the case. This means that conditions can be dealt with before they become very serious and this has major benefits for the patient, their family and for the wider community.


